Oral Anticoagulants FAQs
Oral Anticoagulants FAQs
Fill in our anonymous survey and share your thoughts on this resource.
Medicines to prevent stroke when you have atrial fibrillation
This page answers common questions about atrial fibrillation and oral anticoagulants. It covers:
- what they are,
- why anticoagulants are important if you have atrial fibrillation,
- the different types of anticoagulant medicine,
- the risks and benefits of taking anticoagulant medicines, and
- what to know if you have been prescribed an anticoagulant.
Atrial fibrillation is a condition where the heartbeat becomes fast and irregular. This can increase the chances of a blood clot forming. Blood clots that go to the brain can cause a stroke, damaging part of the brain.
Oral anticoagulants are medicines that make it harder for blood to clot. Some people call them blood thinners.
If you are prescribed an anticoagulant, it is important to understand why you need it, how to take it safely and what side effects to watch out for.
Medical words that are good to know when reading this information.
Active ingredient: The active ingredient is the chemical in a medicine that makes it work.
Arrhythmia: Arrhythmia is when you have problems with your heartbeat. It might beat too fast or too slow, or in an irregular pattern. This means it does not beat in a steady pattern.
Atrial fibrillation (AF): Atrial fibrillation is a type of arrhythmia.
Blood clot: When blood clumps together. Clots can help slow blood flow when you have hurt yourself. In some cases, blood clots can cause unwanted damage, like a stroke.
Health professional: Health professionals have the training to help give you medical care. They include GPs, specialists, chemists/pharmacists, nurses, physiotherapists, dentists, Aboriginal Health Workers and Aboriginal Health Practitioners.
Oral anticoagulant (an-tee-koh-AG-yuh-luhnts): A medicine that you put in your mouth (oral) and swallow, to slow down clotting of the blood. They are sometimes called blood thinners.
Stroke: A stroke happens when blood can’t get to a part of the brain. Blood contains oxygen and food for your brain cells. If your brain cells do not get enough oxygen, they die.
Atrial fibrillation (AF) is when your heartbeat speeds up and loses its regular rhythm. For some people, changes to the heartbeat happen in bursts, for others it is most or all the time.
Anyone can get atrial fibrillation, and it can happen at any age.
It is more common as people get older and in those with risk factors like high blood pressure. More than half a million people in Australia are living with atrial fibrillation.
You may get symptoms like palpitations (feeling that your heart is beating too fast or not regularly), dizziness, or shortness of breath, or have no symptoms at all.
Atrial fibrillation affects how the heart pumps blood. Blood that doesn’t flow properly can clot inside the heart. Clots that form this way can break loose and travel through the body. If a clot reaches the brain, it can block a blood vessel and stop blood from getting through. This is called a stroke, which causes damage to the brain. This damage can:
- affect how you talk,
- make swallowing difficult,
- affect how you move,
- change how you think,
- be permanent (lasts forever) or temporary (goes away).
Blood clots are usually a normal part of healing. They stop blood flowing from a blood vessel. When a clot forms in a blood vessel that is not damaged, it can block the normal flow of blood and is dangerous to your health.
Being told you have atrial fibrillation may leave you feeling concerned and confused. But you are not alone. Many Australians have this condition and continue to live busy and active lives. Atrial fibrillation can usually be managed with medicines, a healthy lifestyle and regular medical checks.
The Heart Foundation
The Heart Foundation has general information about atrial fibrillation. This webpage includes a short video that might be of interest to some people (only available in English). Click here to view this resource.
Heart Support Australia
Heart Support Australia has a factsheet that summarises atrial fibrillation and why it is important to treat it. Click here to view the factsheet.

Hearts4Heart
Hearts4Heart have a general information brochure, Atrial Fibrillation (AF) Explained: A guide for people living with an irregular heartbeat. It explains atrial fibrillation, causes and how it is treated. It also has answers to some common questions about the condition. Click here to view the brochure.
Treatment for atrial fibrillation will be different for each person. It is important to talk with your health professional about what your needs are when it comes to treating atrial fibrillation. Some people will need medicines; others might need to have a medical procedure. Choices about treatment will also consider symptoms, the cause, and any other health conditions a person might have.
Overall, there are four main areas of treatment that your health professionals might talk to you about:

- Rate control – these treatments aim to bring the heart rate back into the normal range (60–100 beats per minute).
- Rhythm control – these treatments aim to restore normal rhythm (also called sinus rhythm).
Note: Some people will take medicines to help control their rate or rhythm. Other people may need a medical procedure instead.

- Anticoagulation – these are medicines that can help lower the risk of a stroke by making it harder for clots to form in the heart (see below, ‘what are oral anticoagulants?’)
- Risk factor management – these are other health conditions that make it more likely for a person to develop atrial fibrillation (see below, ‘what else can I do to manage atrial fibrillation?’)

The Stroke Foundation has an information brochure that explains what it is like living with atrial fibrillation. Click here to view the brochure.
Hearts4Heart
Learn more about the different types of treatments for atrial fibrillation at Hearts4Heart. Click here to read more.
Taking care of your heart and general health is an important step in managing atrial fibrillation. This includes helpful actions such as:
- Being a healthy weight
- Stopping smoking
- Reducing alcohol
- Staying active
- Keeping other health conditions in control – such as blood pressure and cholesterol levels.
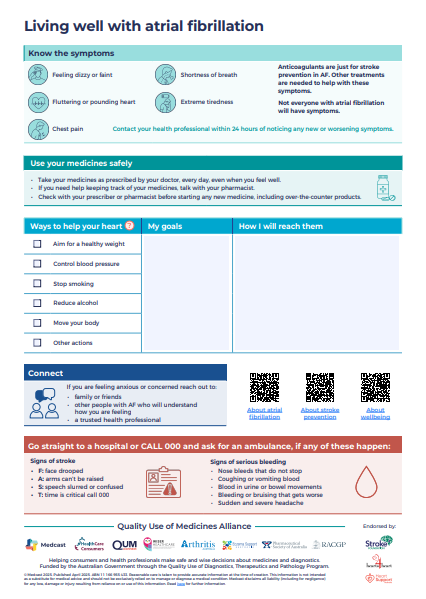
To find more information about living well with atrial fibrillation, read the Anticoagulants Care Plan.
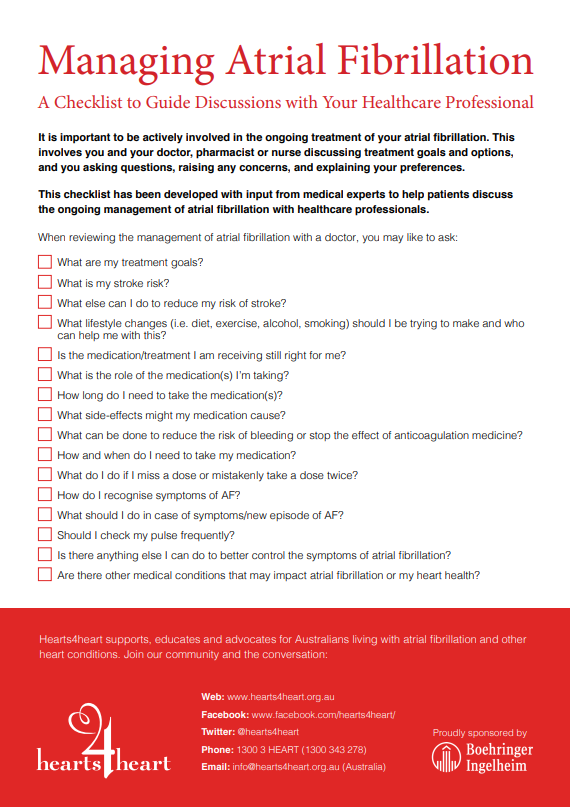
Hearts4Heart
Hearts4Heart have prepared a checklist to help you discuss ongoing management of your condition with healthcare professionals. Click here to view the checklist.
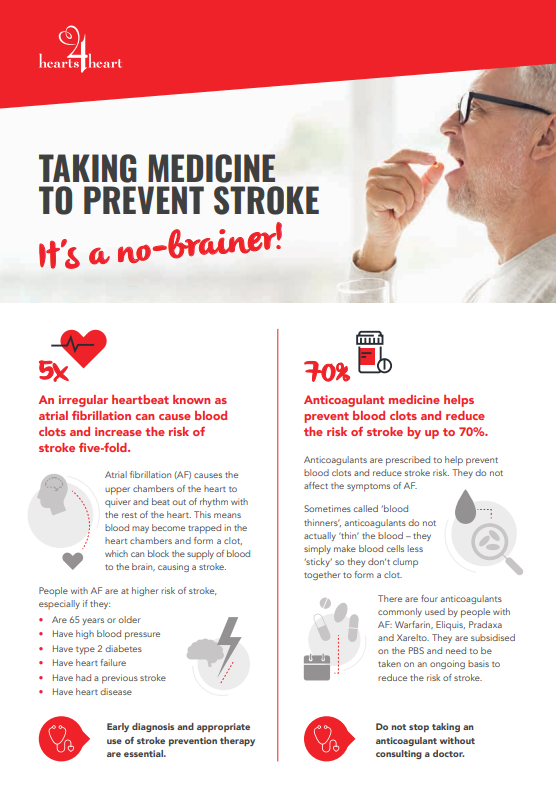
Atrial fibrillation is a major cause of stroke in Australia. Research shows that the risk of stroke is up to five times greater in people who have atrial fibrillation than in people who do not. This is because atrial fibrillation affects the heart’s ability to pump blood effectively.

This can lead to blood pooling and make it more likely that a clot will form. If a clot travels up to your brain, it can block the blood flow and cause a stroke.
If you have atrial fibrillation, your doctor or specialist can check your stroke risk and prescribe the most suitable treatment (like an anticoagulant medicine) to help keep you safe. Even if you feel fine, atrial fibrillation still raises your stroke risk, so acting early and getting the right treatments is best.
Clots can also travel through other blood vessels in your body and block blood flow to your arms or legs, or even one of your vital organs (like your lungs). So, taking an anticoagulant may have other benefits too.
If you have atrial fibrillation, your risk of stroke may be higher if you:
- Are 65 years or older
- Have high blood pressure
- Have type 2 diabetes
- Have heart failure
- Have had a previous stroke
- Have heart disease
The best action you can take is to ask your doctor to check your stroke risk. Even if you feel fine, acting early and getting the right treatments for you is best.
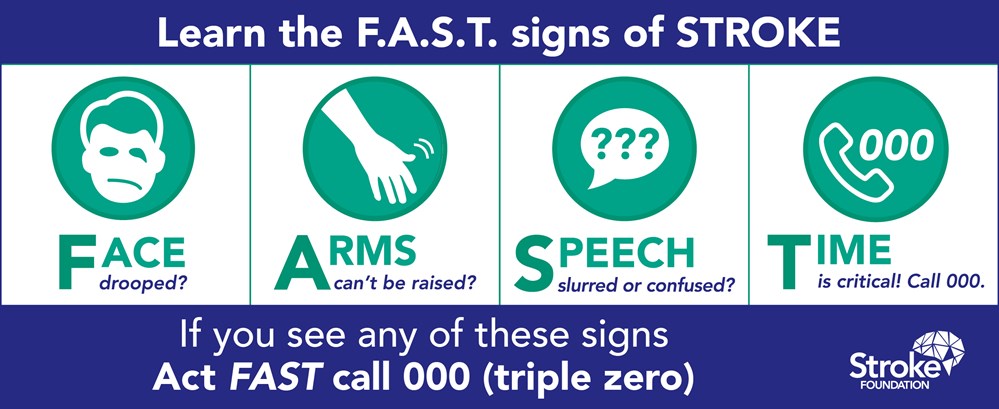
Image from https://strokefoundation.org.au/about-stroke/learn/signs-of-stroke
The Stroke Foundation have more information to explain stroke and what else you can do to prevent them. Click here to learn more.
Oral anticoagulants are sometimes called blood thinners, but they don’t make the blood thinner. Instead, they work by slowing down the body’s clotting process. This helps prevent harmful blood clots that can cause a stroke, while still allowing the blood to clot when needed for minor injuries like a nosebleed.
You are taking an anticoagulant if your medicine has one of these active ingredients in it:
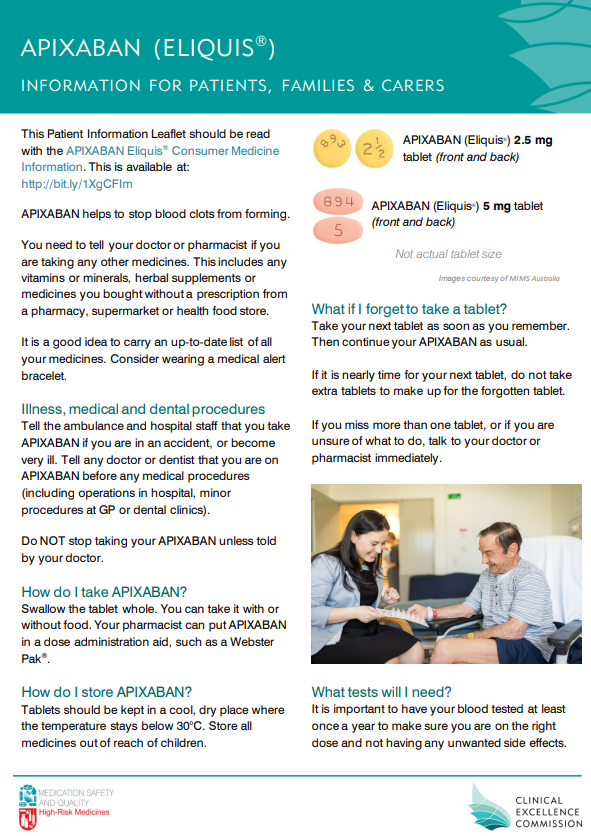
- Apixaban (a-pix-a-ban)
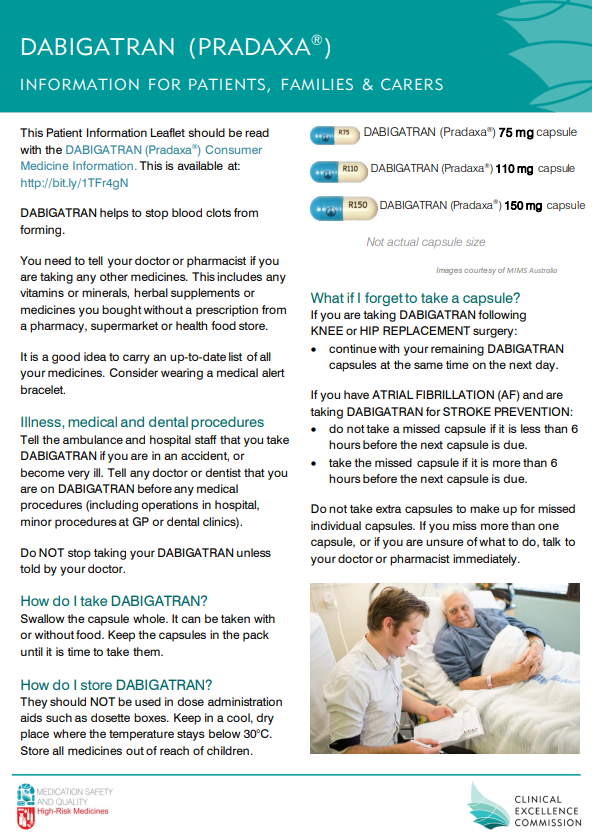
- Dabigatran (da-big-a-tran)
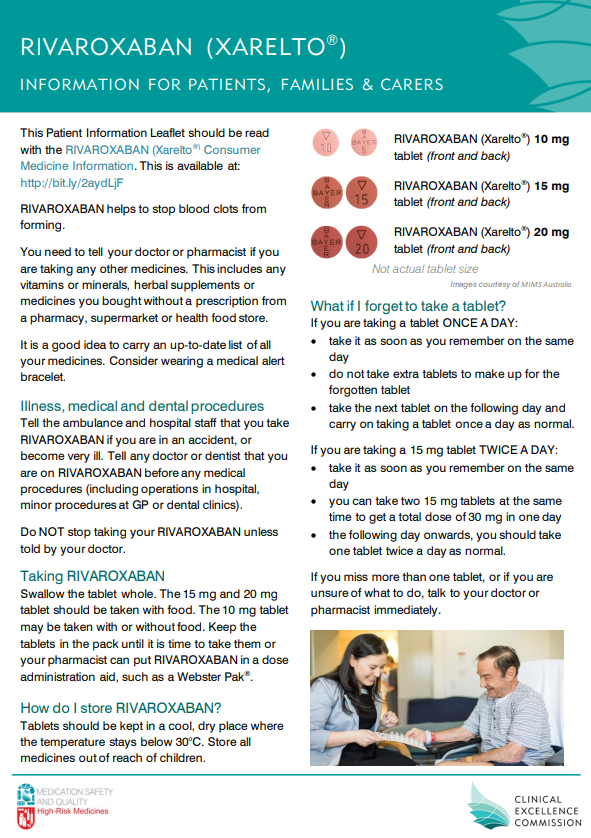
- Rivaroxaban (ri-va-roks-a-ban)
- Warfarin (waw-fuh-rin)
Apixaban, dabigatran and rivaroxaban are also known as ‘DOACs’ (direct-acting oral anticoagulants). Patient information sheets for these three medicines can be found in English and 5 other languages from the NSW Health Clinical Excellence Commission. Click here to go to their webpage.
Healthdirect
More trusted information about your medicine can be found at Healthdirect’s medicines information page. Type the active ingredient (apixaban, dabigatran, rivaroxaban or warfarin) into the Medicines information search bar.

Western Australian Department of Health
The Western Australian Department of Health has prepared a booklet for people taking apixaban, dabigatran or rivaroxaban. It covers information about taking your anticoagulant, possible side effects and how to store it. Click here to view this resource.
Western Australian Department of Health
The Western Australian Department of Health has prepared a booklet for people taking warfarin. It covers information about taking your anticoagulant, possible side effects and how to store it. Click here to view this resource.
Many people who have atrial fibrillation take an anticoagulant every day. This helps to lower the risk of stroke.
People with atrial fibrillation also need other treatments to help their heart health and control abnormal heartbeats.
All medicines have benefits (good outcomes that help our health) and unwanted effects (also called side effects).
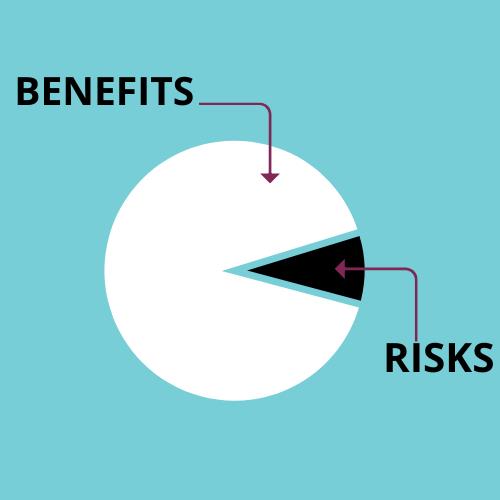
Side effects from taking an anticoagulant are increased risks of bleeding and bruising.
Serious internal bleeding (such as in the gut or brain) can happen but is rare.
These side effects need to be balanced against the benefit of lowering stroke risk. The benefits of preventing a stroke with an anticoagulant almost always outweigh the risk of bleeding.
Hearts4Heart
Read what Hearts4Heart say about taking an anticoagulant when you have atrial fibrillation. Click here to view this resource.
If you take an anticoagulant, it is important to use the medicine safely and correctly. Examples of anticoagulants include apixaban, dabigatran, rivaroxaban and warfarin.
Before you start taking your anticoagulant medicine for the first time, your doctor will do a blood test and check the health of your liver and kidneys (often described as liver function and kidney function).
Your doctor will need to check your kidney function at least once every year, and re-check it if your health condition or medicines change.
If you take warfarin, your doctor or nurse will organise routine blood tests to monitor how it is working.
While you are taking anticoagulants, you will need to take care with activities that could lead to injury or cause bleeding. Talk with your health professional about actions you can take to reduce the chance of bleeding or bruising. This might include:
- using gloves in the garden,
- changing the type of razor you use for shaving, or even
- using a softer toothbrush so you do not hurt your gums when brushing your teeth.
You should contact your health professional immediately and get urgent medical attention if you have:
- Nose bleeds that do not stop
- Coughing or vomiting blood (may look like soil/ coffee grind)
- Blood in urine or bowel movements (may look dark like tar)
- Bleeding or bruising that gets worse
- Sudden and severe headache
- Take the anticoagulant exactly as prescribed and at the same time every day.
- Know what to do if you miss a dose.
- Make sure all your health professionals know you are taking an anticoagulant. This includes your blood collector, dentist, dietitian, GP, nurse, pharmacist, physiotherapist, podiatrist and specialist. A medicines list can be a useful way to keep all the information about your medicines together.
- Use a medical alert card or bracelet.
- Check with a health professional before taking any new medicines, in case there is a risk of interactions. This includes non-prescription and complementary medicines such as herbs and vitamins.
- If you are specifically taking warfarin, NPS MedicineWise have some extra tips. Do not stop taking your anticoagulant without talking to your prescriber first. Stopping can put you at increased risk of developing a blood clot.
- You can find more information about taking an anticoagulant when you have atrial fibrillation in the Anticoagulants Care Plan.
The NSW Health Clinical Excellence Commission
The NSW Health Clinical Excellence Commission has a patient information leaflet for apixaban in the following languages:
The NSW Health Clinical Excellence Commission
The NSW Health Clinical Excellence Commission has a patient information leaflet for dabigatran in the following languages:
The NSW Health Clinical Excellence Commission
The NSW Health Clinical Excellence Commission has a patient information leaflet for rivaroxaban in the following languages:
Western Australian Department of Health
The Western Australian Department of Health has prepared a booklet for people taking warfarin. It covers information about taking your anticoagulant, possible side effects and how to store it. Click here to view this resource.